SPOTLIGHT OP-ED
Why I became a nurse in an underpaid, hostile environment that needs to be fixed
Rene Sparks qualified as a nurse 21 years ago. Now, on International Nurses Day, she reflects on her journey and what’s needed to ensure a better future for nursing in South Africa.
Today we celebrate nurses as we do every year on 12 May. The International Council of Nurses proclaimed this year’s slogan as “Our Nurses, Our Future”, but what is the future of nurses in South Africa?
At the height of the Covid-19 pandemic we saw a huge campaign launched by the World Health Organization, uplifting the stature of nurses and midwives and showcasing them as the backbone of health systems at a global level. In the South African context, the story goes that they will also be central to the health system once National Health Insurance is implemented, yet there are many red flags raised as we continue the planning discussions in preparation for this change with little to no answers about that future.
‘I will never be a nurse’
By the time my mother had to decide on a career, nursing was one of those professions that provided stability and security to black and coloured women during apartheid. You had two choices – become a nurse or a teacher. That’s how my mother began her nursing journey, but she was so passionate about it that it would probably have been her choice, regardless.

The South African Nursing Council notes that 47% of the nurses on its database are older than 50. (Photo: GCIS)
Her passion was not what spurred me on to become a nurse, though. I looked at her long hours and tireless devotion to her community and the mental health fraternity and literally uttered the words: “I will never be a nurse.” Then I met a young staff nurse during a youth weekend away. She was so proud of her profession. She just oozed pride, and at that moment, I went from a potential engineering student to a nursing student.
My father was livid. He could not comprehend why his only daughter would observe the work hours of her mother and still choose to become a nurse. But in many ways, I believe nursing chose me. Once I made the decision, I never looked back. I remember being mocked and berated for my choice in social circles, but feeling a deep connection to this calling.
I have not entered it blindly though. I was aware of my privilege and the weight of caring for people at their most vulnerable. The experiences I have made while holding the hand of someone taking their last breath, supporting a mother delivering a stillborn baby, engaging with my first person living with HIV, and watching someone slip away after a huge battle with cancer have been deeply embedded in my consciousness. I do not believe these experiences to be without life-altering potential and believe they have shaped me into the healthcare worker I am today.
Threats to nurse autonomy
It is often believed that nurses are the handmaidens to the doctor and we should not think but do. Those sayings were so wrong, but even today, the inferiority of the quality of nurse training, lack of supervision and very limited mentoring all threaten the autonomy of the nurse.
Nurses, despite having a day and even a week dedicated to celebrating them, are still, for the most part, underpaid, overworked and professionally stunted. By stunted I am referring to the lack of mandatory continuous professional development and upskilling. Somehow, as the backbone of primary healthcare, they are often unable to take time out for much-needed training.

As NHI looms, the threat that nurses will be ill-equipped to render quality healthcare services is a glaring reality. (Photo: Rosetta Msimango / Spotlight)
One often hears of nurses being rude and impatient. Though some may very well display these horrible traits, for the most part, people have entered this profession to improve healthcare services to individuals, families and communities at large. In my 21 years of experience, the issue is hugely exacerbated by the healthcare system, which does not support nurses. The hours are long and gruelling – exacerbated by staff shortages in facilities. The environment is hostile, the workload unequal and the pay shoddy. Many nurses find themselves moonlighting to make ends meet.
Advocate for us
Though not an excuse for unprofessional behaviour, I do want activists and health advocates to fight for better working conditions, upskilling opportunities and a larger workforce in our public health sector.
The mental health of our clients and communities appears topical at the moment, but what about the nurse? The trauma of loss, observation of patient suffering and abuse by many of the actors in the health space can take their toll on the mental health and well-being of our nurses, too. When we plan for the public, we must remember to include the healthcare workers and their health and well-being.
This is even more critical now as we embark on establishing the National Health Insurance (NHI) system.

Nurse Ncikazi Tsotsi at the NHI public hearing in Gqeberha in 2019. (Photo: Black Star / Spotlight)
As NHI looms, the threat that nurses will be ill-equipped to render quality healthcare services is a glaring reality. The South African Nursing Council (SANC) notes that 47% of the nurses on its database are older than 50. This narrative of ageing nursing personnel started years ago and if we had a proactive plan to address this, South Africa may in fact have had a fighting chance to implement NHI smoothly.
In a damning article published in February, the Democratic Nursing Organisation of South Africa highlighted that the South African public health sector has a deficit of 27,000 nurses and yet there are 5,000 currently unemployed. How can this be acceptable? It further noted that the South African government has placed certain nursing specialities on a scarce skills list in the hope of recruiting from other countries instead of planning to upskill and uplift domestically.
Part of me wants to speak about accountability, collaboration and change management, but the other part bleeds for nurses as the workload and responsibilities increase and the work environment becomes more hostile. All this makes it hard to see the silver lining.
I do, however, believe that if the South African Nursing Council and National Department of Health actually engage the people on the ground, those at the coalface, those with expertise, and review their current implementation plans, they will see the same glaring gaps that we see every day.
There must be a call to action for all nursing leadership, nursing activists, nurses and nursing education establishments to collectively take a stand and demand that we revise our current approach to the nursing curriculum and work on making nursing more appealing to young people. This could be one step in the right direction.
When I qualified as a nurse, it was a four-year course. The nursing degree I completed included community nursing, psychiatric nursing, general nursing and midwifery, and although I might not practise it all, I am able to fall back on that knowledge during client or patient engagements. Now it is a five-year course with one qualification, with the nurse trained as a generalist. The fear is how does that serve our communities? We need midwifery, for example, to do Nimart (initiate people on HIV treatment) and you need community nurses to be working in primary healthcare. If you come out with one general qualification, how exactly will this pan out?
We need a rethink on how we train nurses and how we can strengthen the curriculum so that we can get nurses who can address HIV and all issues in primary healthcare. In my programme, HIV testing, for example, nurses don’t get trained in HIV testing. It is just monkey see, monkey do and unfortunately that doesn’t translate into quality service.
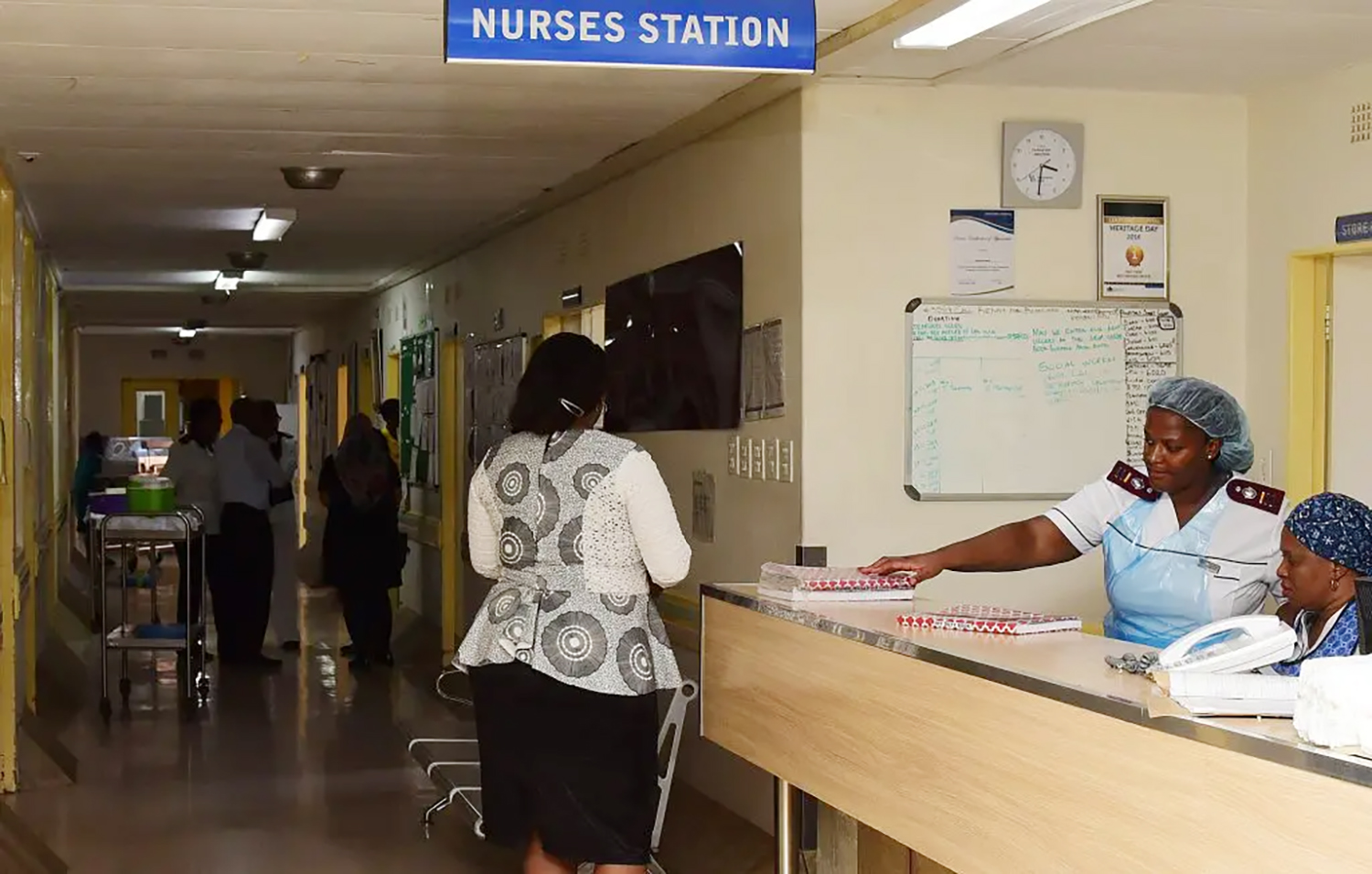
According to the Democratic Nursing Organisation of South Africa, the South African public health sector has a deficit of 27,000 nurses yet there are 5,000 currently unemployed. (Photo: Denvor de Wee / Spotlight)
Very often nursing practice is see one, do one, and then you’re the expert. I’m arguing that these things must be part of the curriculum. For example, why must a nurse come out of nursing school and then only learn IMCI (Integrated Management of Childhood Illness)? Why is IMCI not being done practically in the facility and the theory in class, as part of the curriculum?
Nurses today are expected to know everything, which is impossible, but we are not upskilling them and making sure the curriculum is so robust that it addresses all disease profiles and our communities’ healthcare needs. We are talking about integrative and holistic healthcare, so we cannot be training nurses only in one way. There is a malalignment of what our communities need and what nursing schools are churning out.
We must fix that.
We need an urgent change in the curriculum of nurses to ensure we can support the needs of the health system and communities, build great leadership for the future and ensure quality health services for all. DM/MC
Sparks is a nurse, health equity advocate, and Tekano and Aspen New Voices Fellow with 21 years’ experience working across South Africa with a focus on ensuring equitable and just access to quality healthcare for all. She is also a Quote This Women + Voice of the Year Award Winner.
This article was published by Spotlight – health journalism in the public interest.

















 Become an Insider
Become an Insider
Comments - Please login in order to comment.